Author: Benjamin Krynski – Paramedic | Co-Founder Real Response
History:
The management of heat stroke has been recorded as far back as 24BCE, when Roman soldiers were told to drink olive oil and wine while rubbing both into their bodies in response to overheating(1). In the 1500s, physicians recommended tactile stimulation and bloodletting to release internal heat(1). In modern times, Hyperthermia is categorised into three stages, heat stress, heat exhaustion, and heat stroke(5, 6).
Definition:
Heat stroke is the most severe form of hyperthermia and often defined as a “life-threatening condition when the core body temperature exceeds 40oC and there is Central Nervous System Dysfunction (CNS) (1-4).
Exertional Heat Stroke (EHS):
This is the most common form of heat stroke and results from prolonged activity in a hot environment. It may also result from cocaine or amphetamine use as well as status epileptics(5, 6)
Non-Exertional Heat Stroke (NEHS):
Common in the young and elderly and most often occurs during heat waves. NEHS is also known as classical heatstroke(5, 6)
This flowchart illustrates the dynamic cascade and physiological changes during a heat stroke incident(8).
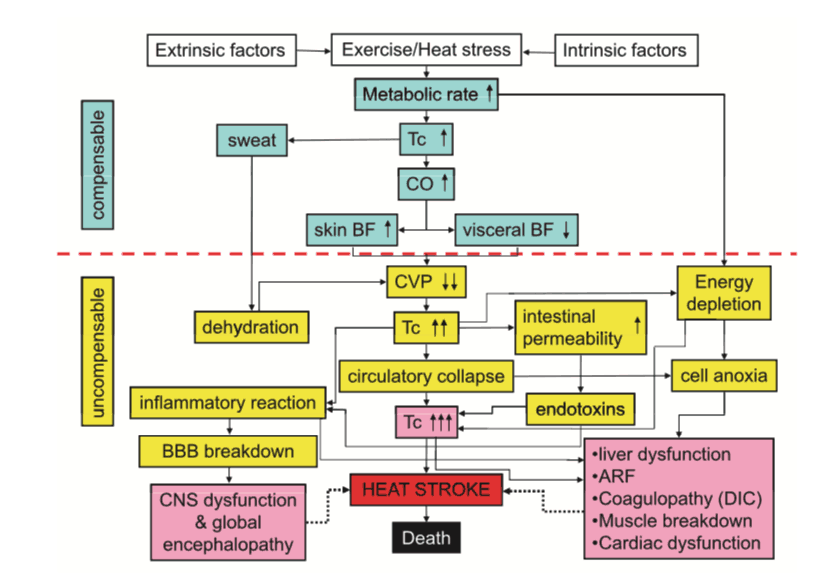
Compensatory phase:
During this phase, the body is able to effectively respond to an increase in core temperature. Peripheral and hypothalamic thermal receptors increase cardiac output, vasodilate skin blood vessels and stimulate the sweat glands. Heat is transferred out of the body through radiation and evaporation. Assuming the person has adequate skin blood flow this system should be effective(8).
Acute-phase-response:
As heat stress progresses the body cells are at risk of denaturation. initially, the body reacts by protecting the cells by inhibiting the heat shock proteins.
This:
1) Prevents disaggregaton of denatured proteins Assist in protein refolding
3) Slows the loss of epithelial integrity
3) Prevents endotoxin leakage
4) Slows hypotension in an attempt to reduce cerebral hypoperfusion.
Uncompensable Phase:
When the body systems can no longer maintain adequate cooling heatstroke becomes uncompensated and may lead to:
• Circulatory failure,
• Hypoxia,
• Increased metabolic demands,
• Cell suppression
• Systemic inflammation
• Failure of the coagulation system.
• Rhabdomyolysis
• Acute Renal Failure
• Disseminated intravascular coagulation
• Death(8)
During this period fluid loses may reach 1-2L an hour and fluid is transferred from the intravascular space to the interstitial space and the total blood volume significantly decreases. As the central venous pressure is reduced, there is an inability to transfer heat to the extremities and muscle damage can occur due to ischemia. This may cause Rhabdomyolysis and acute renal failure. Lowered circulation to the gut causes hyperpermeability, increases anaerobic respiration and reduced hepatic function, all assisting in increased acidosis(8).
Concurrently, damage to the cell membranes allows endotoxins into the vascular space creating an endotoxin-modulated shock syndrome with associated hypotension, tachycardia and organ hypoperfusion. In addition, the endotoxins release inflammatory cytokines further increasing the action of the inflammatory cascade leading to disseminated intravascular coagulation(8).
Without rapid and effective action this is irreversible.
| Assessment: A rapid assessment of a heatstroke victim must be made and differential diagnosis of other conditions that may cause an altered conscious state. These include but not limited to: • Stroke • Hypoglycemia • Syncope • Intoxication • Electrolyte imbalances Once they have been reasonably excluded, conscious state and internal temperature must be taken. The gold standard for temperature assessment is via a rectal thermometer which is rare outside a hospital environment. Sweat and air may affect axilla temperature measurements which may lead responders to a false sense of security. If someone is suspected to have heatstroke an oral/infrared temperature measurement should not be relied on(5). Responders should look for: • CNS dysfunction • Diaphoresis • Restlessness • Coma • Hallucinations • Confusion • Delirium • Dysarthria (5) |
First Aid:
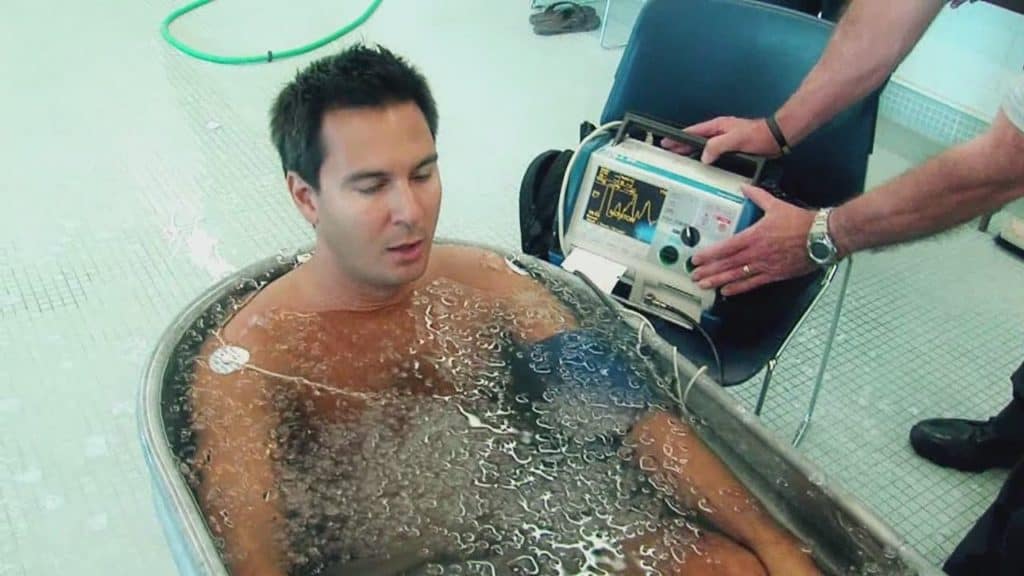
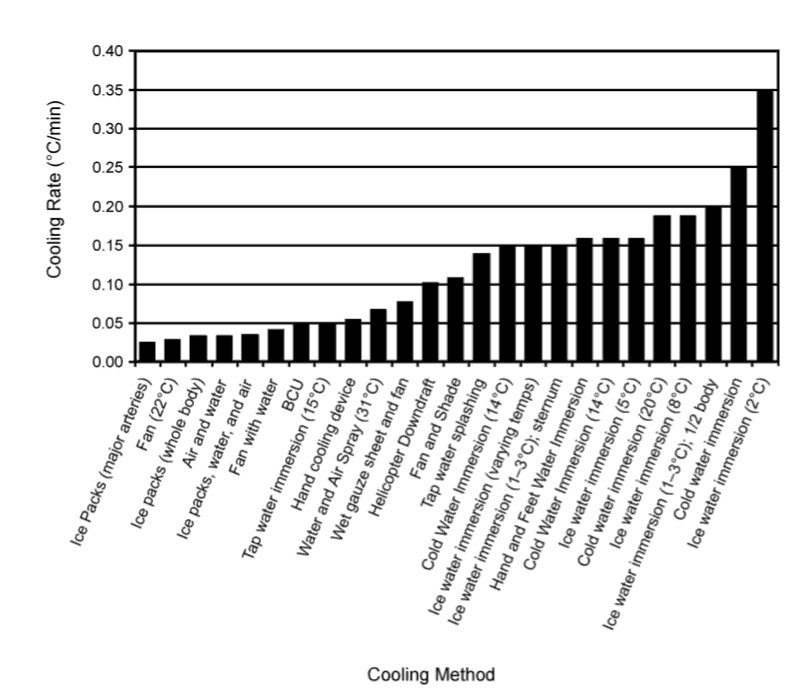
Rapid cooling must be the first step of heatstroke management(4, 5, 7). This includes moving the victim out of the exposure, turning on an air conditioner, removal of their clothing, placing ice packs in the groin, under the armpits, dousing them with water and fanning(2, 9). The gold standard for cooling a heat stroke victim is through cold-water immersion (CWI). However, this is not always possible(1, 2, 5, 10). If CWI is initiated early the victim has near to a 100% survival chance.
Once the victim is cooled to bellow 40oC, cooling should be ceased due to the risk of hypothermia and causing shivering(1, 10).
Advanced Life Support (ALS):
Advanced life support practitioners arriving at the scene should first focus on first aid, being rapid cooling. Cooling should be prioritized over quick evacuation due to the otherwise transport delays until adequate cooling would be established in a definitive care unit(1, 2).
ALS care should include:
• Basic and advanced airway management
• Cool IV fluids through a large vein treating hypovolemia and dehydration
• High flow Oxygen
• Management of seizures if present
• Management of hypoglycemia if blood sugars are low
(1, 2, 5)
References:
1. Bouchama Abderrezak, Knochel P James. Heat Stroke. The New England Journal of Medicine. 2002;346(25):1978-88.
2. Wagner Christopher, Boyd Kathy. Pediatric Heatstroke. Air Medical Journal. 2008;27(3):118-22.
3. Sheng keng Chew, Latif abdul kursi Abdul. A case of heat-related illness. Journal of Paramedic Practice. 2010;3(1):32-3.
4. Casa J Douglas, McDermott P Brendon, Lee C Elaine, Yeargin W Susan, Armstrong E Lawrence, Maresh M Carl. Cold Water Immersion: The Gold Standard for Exertional Heatstroke Treatment. Exercise and Sport Sciences. 2007;35(3):141-9.
5. Nelson Nicolas, Collins Christy, Comstock Dawn, McKenzie Lara. Exertional Heat-Related Injuries Treated in Emergency Departments in the U.S., 1997–2006. American Journal of Preventive Medicine. 2011;40(1):54-60.
6. Flouris D A, Friesen J B, Carlson J M, D CJ, Kenny P G. Effectiveness of cold water immersion for treating exertional heat stress when immediate response is not possible. Scandinavian Journal of Medicine & Science in Sports. 2015;25:229-39.
7. Zeller Lior, Novack Victor, Barski Leonid, Jotkowitz Alan, Almog Yaniv. Exertional heatstroke: clinical characteristics, diagnostic and therapeutic considerations. European Journal of Internal Medicine. 2011;22:296-9.
8. Epstein Y, Roberts O W. The pathopysiology of heat stroke: an integrative view of he final common pathway. Scandinavian Journal of Medicine & Science in Sports. 2011;21:742-8.
9. Douglas CJ, Armstrong E Lawrence, Kenny P Glen, O’Connor Francis G, Robert. HA. Exertional Heat Stroke: New Concepts Regarding
Cause and Care. Current Sports Medicine Reports. 2012;11(3):115-23.
10. Nick B. Exertional heat stroke: a rapidly progressive pre-hospital presentation
Nick. Journal of Paramedic Practice. 2010;4(9):549-50.
11. WEWS News Channel 5. Survival guide: Cold water rescue 2013 [Available from: https://i.ytimg.com/vi/A0jVcKI8kCc/maxresdefault.jpg.
12. DanceSafe. Heatstroke: DanceSafe; 2016 [Available from: https://dancesafe.org/wp-content/uploads/2014/02/heat-stroke.jpg.

