Written By Lydia Muller – First Aid Instructor Real Response
Background
My motivation for writing this article has come from a common question I receive in most first aid classes.
““How do you know if the casualty is or is not breathing normally?”
This seems simple on face value, but telling the difference between normal breathing, and what is referred to as agonal breathing, or Cheyne-Stokes can be very difficult, even for medical professionals. Not to mention involuntary limb movements which may present and further confuse the responder.
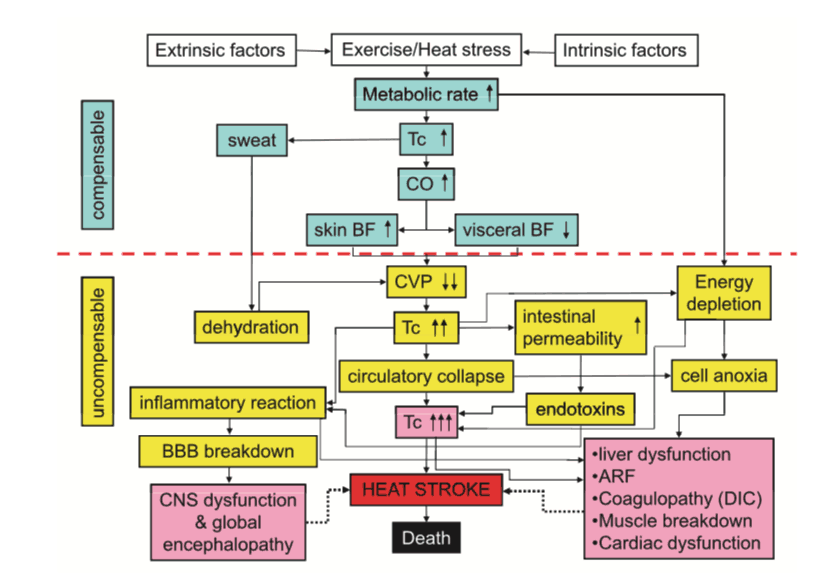
Pathophysiology
When someone’s heart stops (cardiac arrest) that the casualty is still breathing. This is due to a reflex initiated within the brainstem that causes something known as agonal breathing. Agonal breathing is defined as an abrupt and sudden effort to breathe which is ineffective and appears like the person is gasping. It is the final respiratory pattern before breathing stops (respiratory arrest), sometimes known as Cheyne-Stokes(8, 9).
Several studies undertaken of Triple 0 (Australia’s emergency service number) indicated that agonal breathing was witnessed in 40% of cardiac arrests, 55% of these were witnessed arrests.
Agonal breaths were present in 18.4% of all cases considered in these studies (witnessed and unwitnessed). The reality of being a first aider is that you are much more likely to see agonal breaths than the first responders/paramedics arriving later on(8).
Involuntary Limb Movements
Involuntary limb movements is another major factor that contributes to delayed CPR. This phenomenon is caused by a lack of blood supply to the brain leading to hypoxia. Within the first few minutes of cardiac arrest, the limbs may exhibit seizure-like movements and appear to be reaching away from, or localizing towards the center of the patient’s chest. On very rare occasions, the patient can even appear to be combative towards the first responder. This type of movement is often seen alongside agonal breathing(5, 7, 10).
The Problem
The issue is that agonal breathing often confuses the rescuer delaying the initiation of CPR (by both first raiders and professionals). In fact, studies have shown that a bystander is far more likely to commence CPR in an unwitnessed cardiac arrest than if they were present when the casualty lost consciousness (4). This is likely to be leading to poorer patient outcomes as every moment CPR is delayed is longer the brain is starving of oxygen.
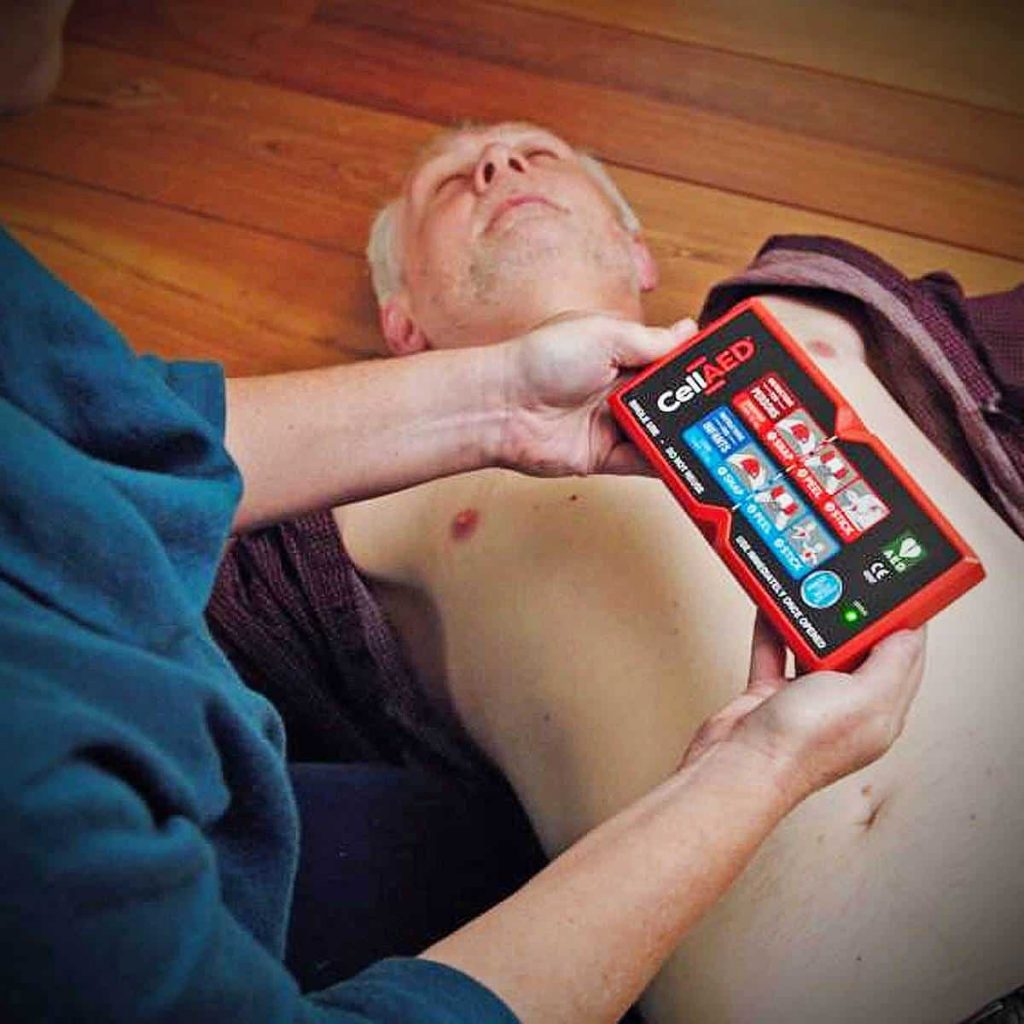
The Solution
When conducting your primary survey (DRSABCD) you should ensure that you take your time and check Response and Breathing properly (10-sec look listen and feel), if you are still unsure, take even a little bit extra time or ask someone else their option. If you are still unsure then continue with CPR. Do your best not to let agonal breaths or involuntary movements delay you from starting CPR. However, if it does, it’s ok. It happens to professionals regularly.
*Note during the COVID-19 pandemic only look and feel, do not bring your face close to the patients to listen to breathing.
CASE STUDY
Written By: Benjamin Krynski Title: Paramedic / Director of Training at Real Response
Afternoon shift – Advanced Life Support (ALS) Ambulance Major Metropolitan Centre
Call: 67 year old woman who was feeling weak in a hairdresser.
On Arrival: We arrived to see a 67 year old woman in a hairdresser, stating she was feeling weak and nauseous. She was with her daughter who was quite worried. There was no history of cardiac disease, and there were no events leading up to her presentation.
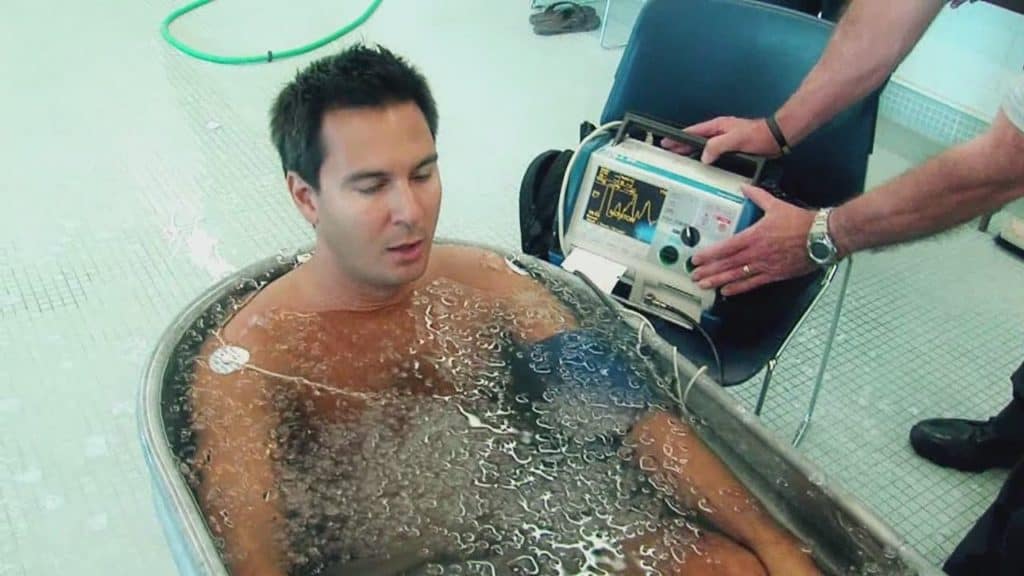
On Examination: Patient was pale, clammy, weak, unable to open her eyes without a physical stimulus. I went to take a BP on her R arm and could not hear anything, I went to try the left arm, and as I was taking the cuff off the R arm and moving it to the L, I noticed she slumped forward and stopped responding. I went and applied strong pain stimulus and there was no response, I checked breathing, she was not breathing, I felt for a carotid pulse (ALS skill only) and there was none. I told my partner to set up the defibrillator, and with a bystanders help moved her to the ground to start CPR. As she was moved onto her back, she started breathing, but it was strange, only one breath every so often, and it was more of a gasp combined with her arms spasming up. My partner looked at me and said “is she breathing”. Second guessing myself I went to re-check breathing and pulse and confirmed there was no normal breathing and we commenced CPR.
Treatment: We administered a total of 10min of CPR, no shocks. By this time a second crew had arrived and we had started our ALS cardiac and airway procedures. As we were about to perform an advanced airway procedure the patient started breathing spontaneously, and 2min after this regained consciousness. She was in quite a lot of pain as we had broken several ribs during chest compressions.
Outcome: 6 hours later I returned to the hospital we had transported her too and she was sitting upright in bed with an oxygen mask on, high on pain meds with her family around her. She held our hands thanking us.
Final Thoughts: Agonal breaths will delay you initiating CPR and will make you double guess yourself. This is ok, just not let it delay you more than a few seconds. CPR works! Especially if you witness the person collapsing.
Summary
The term agonal breathing generally refers to intermittent gasping respirations. However, within the context of first aid, agonal breathing simply refers to abnormal breathing patterns and sounds.
Including:
- Gasping
- Wheezing
- Groaning
- Snorting
- Snoring
- Gurgling
- Weak breathing (i.e. rapid shallow breaths)
- Occasional breath
When assessing breathing in the B of the primary survey you may notice these and still feel unsure.
Assess the global picture and if the person is also blue, pupils dilated and still then you likely need to start CPR asap. You can always use the 000 caller for guidance. If unsure it’s better to start CPR than not.
Further Information
This link provides a good example of what agonal breaths and involuntary limb movements look like during cardiac arrest.
If you have any questions please feel free to reach out to us via our social channels and we will be happy to answer any questions.
References
- Alfsen, D., Møller, T. P., Egerod, I., & Lippert, F. K. (2015). Barriers to recognition of out-of-hospital cardiac arrest during emergency medical calls: a qualitative inductive thematic analysis. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine, 23(1), 70. https://doi.org/10.1186/s13049-015-0149-4
- Australian Resuscitation Council. (2016). ANZCOR Guideline 5 – Breathing. Retrieved 20 August from https://resus.org.au/guidelines/
- Ball, S., Riou, M., Gallant, S., Whiteside, A., Bailey, P., & Finn, J. (2018). 26 The influence of agonal breathing on call-taker recognition of out-of-hospital cardiac arrest. BMJ Open, 8(Suppl 1), A10. https://doi.org/10.1136/bmjopen-2018-EMS.26
- Brinkrolf, P., Metelmann, B., Scharte, C., Zarbock, A., Hahnenkamp, K., & Bohn, A. (2018). Bystander-witnessed cardiac arrest is associated with reported agonal breathing and leads to less frequent bystander CPR. Resuscitation, 127, 114-118. https://doi.org/https://doi.org/10.1016/j.resuscitation.2018.04.017
- Kramer, E. B., Serratosa, L., Drezner, J., & Dvorak, J. (2016). Sudden cardiac arrest on the football field of play—highlights for sports medicine from the European Resuscitation Council 2015 Consensus Guidelines. British Journal of Sports Medicine, 50(2), 81. https://doi.org/10.1136/bjsports-2015-095706
- Ng, Y. Y., Leong, S. H. B., & Ong, M. E. H. (2017). The role of dispatch in resuscitation. Singapore medical journal, 58(7), 449.
- Olaussen, A., Nehme, Z., Shepherd, M., Jennings, P. A., Bernard, S., Mitra, B., & Smith, K. (2017). Consciousness induced during cardiopulmonary resuscitation: An observational study. Resuscitation, 113, 44-50. https://doi.org/https://doi.org/10.1016/j.resuscitation.2017.01.018
- Roppolo, L., Pepe, P., & Bobrow, B. (2010). The role of gasping in resuscitation. In Intensive care medicine (pp. 83-95). Springer.
- Smereka, J., Szarpak, Ł., Czyzewski, Ł., Zysko, D., & Smereka, A. (2016). Are physicians able to recognition ineffective (agonal) breathing as element of cardiac arrest? The American journal of emergency medicine, 34(6), 1165.
- Zorzi, A., & Corrado, D. (2018). Cardiac arrest during sports activity is difficult to recognise? Let the AED do the job! Netherlands Heart Journal, 26(4), 226-227. https://doi.org/10.1007/s12471-018-1097-1